159 North 3rd Street
Macclenny, Florida 32063

Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
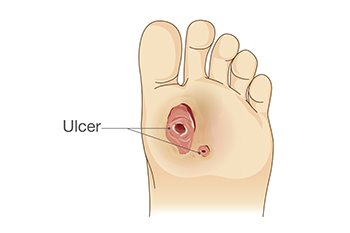
A foot ulcer is defined as any break in the skin. It is the most common type of diabetic foot wound and can lead to loss of functioning and severe complications. These foot wounds often result from factors such as poor blood sugar control, diabetic peripheral neuropathy, and abnormal foot mechanics due to deformities. Diabetic peripheral neuropathy, a side effect of diabetes, can also lead to a loss of protective sensation in the feet, making early injury detection challenging. The assessment of the diabetic foot involves a comprehensive foot and body examination. This can consist of assessing risk factors, undergoing a dermatologic and musculoskeletal evaluation, and having neurologic tests that can determine the degree of sensation. Treatment of diabetic foot ulcers includes debridement, wound culturing, and wound dressings. Additionally, it is important to monitor glycemic control and infection control. Their prevention and management are essential to improve the patient’s quality of life. If you have diabetes and have developed a foot wound or any other foot condition, it is strongly suggested that you make an appointment with a podiatrist who can evaluate your situation, and receive the appropriate treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. John L. Coleman from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.

Finding the perfect pair of running shoes is the first step for any beginner embarking on their running journey. Your choice of footwear can significantly impact your comfort, performance, and overall running experience. It may help to have a podiatrist analyze your gait, arch type, and foot shape in order to guide your purchase. Consider where you plan to run most frequently. Different shoes are designed for specific terrains, such as road running, trail running, or even treadmill running. Comfort should be a top priority when trying on running shoes. They should feel snug but not too tight. Make sure there's ample room for your toes to wiggle and breathe. Take your time to try on several pairs and jog around the store to get a real feel for how they perform. Also, remember that running shoes have a limited lifespan, typically ranging from 350 to 500 miles, depending on terrain, running style, and body weight. Keep track of your mileage and be prepared to replace your shoes when they show signs of wear and tear. For more information on finding the right running shoe for you, it is suggested that you make an appointment with a podiatrist.
If you are a runner, wearing the right running shoe is essential. For more information, contact Dr. John L. Coleman from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
To increase performance and avoid the risk of injury, it is important to choose the right running shoe based on your foot type. The general design of running shoes revolves around pronation, which is how the ankle rolls from outside to inside when the foot strikes the ground.
If you have any questions please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Running may seem like a simple to do. However, running is actually a complex movement that puts stress on the ligaments, bones, and joints of the body. Selecting the correct running shoe is important for increasing performance and avoiding risk of injury. Running shoes should be selected based on your foot type. Considerations such as trail versus road shoes are important. Your foot type dictates the degree of cushioning, stability and motion control you require. The most accurate way to learn your foot type is to visit a local shop that specializes in running shoes. Professionals can measure your arch type, stride and gait and help you with your shoe needs.
The design of running shoes is created around the idea of pronation. Pronation is the natural rolling movement of your ankle from the outside to inside when your foot strikes the ground. If you run properly you strike the ground on the outside of your heel and roll in the direction of your big toe before pushing off once more. Pronation is beneficial because it assists the lower half of your body in absorbing shock and storing energy. Those considered neutral runners pronate correctly and do not need running shoes that help correct their form. Neutral runners can choose from a wide variety of shoes, including barefoot or minimal types. However, those who have arch problems or who adopt an incorrect form while running may experience too much or too little pronation. They may require running shoes that offer additional support.
Those who overpronate experience an over-abundance of ankle rolling. Even while standing, those who severely overpronate display ankles that are angled inward. It is not uncommon for them to have flat feet or curved legs. The tendency to overpronate may cause many injuries. Areas that tend to become injured are the knees, ankles, and Achilles tendon. If you find that you have a tendency to overpronate, you should look at shoes that provide extra stability and motion-control. Motion-control shoes are straight and firm. Shoes of this type do not curve at the tip. The restricted flexibility along the middle of the shoe prohibits the foot from rolling too far inward as your foot strikes the ground.
A less common problem is underpronation. Underpronation, also called supination, is when the feet are unable to roll inward during landing. Those who underpronate have feet that lack flexibility and high arches. This prevents any kind of shock absorption, even though it does place less rotational stress on ankles and knees. This added force can cause fractures, ligament tears, and muscle strains because the legs are trying to compensate for the impact. Those who underpronate need shoes with more cushioning and flexibility. If you have a tendency to underpronate, selecting stability or motion-control shoes may cause you more problems by continuing to prevent pronation.

Heel pain is a common complaint that can affect anyone, but it can be particularly challenging for those who are obese. The excess weight places additional stress on the feet, especially the heels, which bear the brunt of the load. This extra pressure can lead to various painful conditions, including plantar fasciitis, heel spurs, and Achilles tendonitis. Plantar fasciitis, in particular, is a frequent cause of heel pain. The plantar fascia, a thick band of tissue that runs along the bottom of the foot, can become strained and inflamed due to the increased weight. Fortunately, there are ways to manage and alleviate heel pain in obese individuals. Weight loss can significantly reduce the pressure on the feet and the pain. Wearing supportive footwear, custom orthotics, and stretching exercises may also help relieve discomfort. It is essential for those struggling with obesity to address their heel pain, as it can hinder mobility and overall well-being. Seeking help from a podiatrist is a crucial step toward finding relief and improving foot health. If you have heel pain and are overweight, it is suggested that you speak with this type of healthcare professional who can help you manage both conditions.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Dr. John L. Coleman from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.

Ankle pain is a prevalent issue that can disrupt daily life and mobility and strike anyone, from athletes to sedentary individuals. To effectively manage and alleviate ankle pain, it's essential to understand the various underlying causes. Ankle sprains, strains, and fractures can often result from sports-related accidents, falls, or missteps. These injuries can damage ligaments, tendons, or bones, leading to pain and swelling. Common sources of ankle pain include osteoarthritis or rheumatoid arthritis, and may lead to chronic ankle pain due to joint inflammation and deterioration. Additionally, nerve compression syndromes, such as tarsal tunnel syndrome, can result in ankle pain, numbness, and tingling sensations. Identifying the specific cause of ankle pain is crucial in establishing effective treatment. A suitable approach for relief may include rest, medications, and in severe cases, surgical intervention. If you have ankle pain, it is suggested that you consult with a podiatrist who can effectively diagnose the cause and guide you toward the treatment that is right for you.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Dr. John L. Coleman from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Macclenny, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankles are joints that connect bones in the feet with bones in the lower leg. They are comprised of bones, ligaments, muscles, tendons, blood vessels, and nerves. The ankle joint allows the foot to move side-to-side, as well as up-and-down.
Ankle pain can be caused by a variety of conditions, but is most commonly due to soft tissue injuries such as ankle sprains and strains.
An ankle sprain occurs when one or more of the strong ligaments that support and stabilize the ankle become overly stretched or even torn if the ankle rolls, turns, or twists awkwardly. Depending on the grade of sprain (mild-moderate-severe), there will be varying degrees of pain, swelling, and restricted range of motion, along with tenderness, bruising, and ankle instability. There may even be an audible popping noise at the moment of injury.
Ankle strains can sometimes produce similar symptoms of pain, swelling, and loss of motion, however, they are due to overly stretched muscles and tendons—not ligaments. Ankle strains may also cause muscle cramps in the feet, calves and shins.
Ankle fractures are another common source of ankle pain and occur one or more of the three bones in the ankle become fractured (broken). These breaks can be stress fractures (due to repetitive stress) or traumatic fractures (due to an acute injury). Depending on where and how severe the fracture is, symptoms can include pain and swelling that can sometimes spread up to the knee, bruising or discoloration, and an inability to bear weight. A visible deformity or exposed bone may occur in severe fractures.
Various forms of arthritis may also cause ankle pain. Rheumatoid arthritis (RA) causes the immune system to attack healthy joints, like the ankle joint, by mistake, causing stiffness and swelling in both ankles. Osteoarthritis occurs when cartilage covering the ends of bones wears down, causing the bones to rub against each other. This results in pain, stiffness, and reduced range of motion in the ankle. Gout is a form of arthritis where excess amounts of uric acid in the bloodstream crystallize and build up on joints, causing severe pain and swelling. Reactive arthritis causes joint pain and swelling in the ankle in response to an infection in another part of the body.
Other forms of ankle pain include bursitis (an inflammation of a cushioning bursa sac between tendons and bone), scleroderma (a thickening of connective tissues), chronic ankle instability (caused by improperly healed ankle sprains), Achilles tendon injuries, flat feet, or an infection in the ankle.